An ascending aortic aneurysm is the enlargement, or ballooning, of the main artery (aorta) that emerges from the heart. The aorta begins at the aortic valve of the heart and first gives off the coronary arteries that supply the heart itself. It then ascends and gives rise to arteries that supply the brain and arms (the carotid and subclavian arteries). The aorta continues behind the lungs, branching off vessels to the internal organs, and eventually splits into two arteries that travel down each leg all the way to the toes.
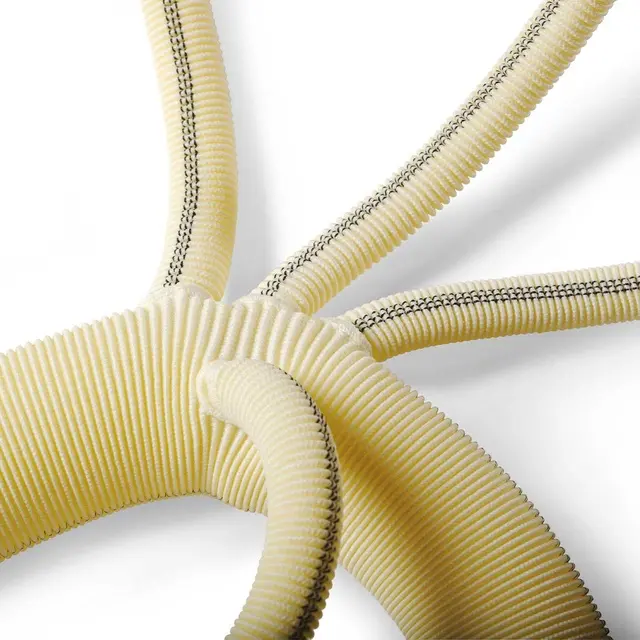
Depending on a person’s height and weight, the normal diameter of the aorta is generally around 2.5 to 3 cm. If the diameter exceeds 5 cm, there is a risk of rupture or dissection, and surgical replacement with a synthetic graft becomes necessary.
However, the decision for surgery is not based solely on the diameter.
- In most cases, the enlargement of the aorta also leads to leakage (regurgitation) of the aortic valve, requiring the valve to be repaired during the aortic replacement.
- If the dilation starts right from the point where the aorta exits the heart, the coronary arteries must be detached from the dilated aorta and reattached to the new synthetic graft—this is known as the Bentall procedure.
- If the valve is to be replaced with a prosthetic one, the valve is replaced and the synthetic graft is sewn beyond the origins of the coronary arteries.
- If the aorta has enlarged up to the branches that supply the brain and arms, the surgical approach changes entirely. In such cases, the entire aorta must be replaced while maintaining cerebral circulation by temporarily stopping the body's blood flow.
All of these conditions should be carefully assessed and planned before surgery using echocardiography and computed tomography (CT), and your surgeon should tailor the operation accordingly.
All the aortic aneurysm surgeries we have described can be performed using a minimally invasive approach. In minimally invasive aortic aneurysm surgery, the entire breastbone is not opened. Instead, only the upper third of the sternum is accessed through a 5 cm incision, allowing the entire operation to be completed.
Because the integrity of the sternum remains largely intact, bone stabilization is significantly better. The smaller incision also enables a faster return to normal life and offers excellent cosmetic results.
- Your doctor should inform you about your condition as if you are hearing about it for the first time, and do so with complete transparency.
- They should discuss all available treatment options—both surgical and non-surgical—and their possible outcomes with you (including medication, monitoring, or surgery).
- If surgery is planned, your doctor should explain the different options and recommend the most suitable one for you (such as valve repair or replacement, mechanical or biological prosthetic valves).
- They should also walk you through the entire process and the associated risks, starting from the preoperative stage.
- Typically, a one-day hospital stay before surgery is required to complete routine preoperative tests. These tests are performed to detect any conditions that may pose a risk during the operation and to take necessary precautions (including detailed blood tests, echocardiography, carotid artery ultrasound, chest X-ray—or CT scan if needed—and a pulmonary function test).
- If you are taking blood-thinning medications, they should be stopped 5–7 days prior to surgery (Aspirin does not need to be discontinued). Your other medications will be adjusted by your doctor.
- Full body shaving will be performed by hospital staff (do not do this yourself; staff will use specialized tools and techniques appropriate for your surgery). Your nurse will explain how to bathe with a special antiseptic soap.
- If your doctor deems it appropriate, a sedative will be given the night before the operation to help you sleep well.
- As you are taken to the operating room, you will be awake but will not remember entering due to the effect of an intravenous medication.
- Heart surgeries are performed under general anesthesia. The anesthesia process takes approximately 45–50 minutes before the surgical procedure begins.
- Electrodes are placed on your back to monitor your heart rhythm throughout the surgery. A small intravenous line is inserted into your arm. A special arterial cannula is placed in your wrist to continuously monitor your blood pressure during the surgery and in the intensive care unit. These steps are painless and will not be remembered due to the sedative injection given before being taken to the operating room.
- General anesthesia is administered through intravenous medications. Once full anesthesia is achieved, a breathing tube is inserted into your windpipe, and your breathing is maintained with a ventilator.
- Heart surgeries are performed under general anesthesia. The anesthesia process typically takes about 45–50 minutes before the surgery begins.
- Electrodes will be placed on your back to monitor your heart rhythm throughout the procedure. A small intravenous line will be inserted into your arm. A special arterial cannula will be placed in your wrist to monitor your blood pressure continuously during surgery and in the intensive care unit. These steps are painless and will not be remembered due to the sedative injection given before being moved to the operating room.
- General anesthesia is administered via intravenous medications. Once full anesthesia is achieved, a breathing tube will be inserted into your windpipe, and your breathing will be maintained by a ventilator.
- A larger IV line will be inserted in your neck to deliver medications and fluids during surgery and the intensive care stay. Blood samples can also be taken from this line, avoiding repeated needle sticks. A urinary catheter will be placed.
- To examine the heart during the operation, especially to evaluate valve function after valve surgery, a special probe will be inserted into your esophagus for echocardiographic imaging.
- Your body will be positioned appropriately for the surgery, and the surgical site will be cleansed with antiseptic solutions.
- The surgery begins… From this point, your surgeon will be assisted by two other surgeons. There will also be two nurses—one in sterile attire and the other on standby in the operating room. An anesthesiologist and a technician will remain by your side throughout. Additionally, two perfusionists will operate the heart-lung machine, which temporarily takes over the function of your heart and lungs during the surgery.
- After the surgery is completed, you will be transferred to the intensive care unit while still under anesthesia and connected to a ventilator.
- You will not wake up in the operating room. Based on your general condition, you will be awakened slowly, safely, and comfortably in the ICU approximately 4–6 hours after surgery (possibly later).
- You will not feel any pain. Pain control will be managed with medications that are started as the anesthesia is being tapered off, and their dosages will be carefully adjusted by the ICU physician.
- One of the most common complaints in the ICU is thirst. Your fluid balance will be carefully maintained with intravenous fluids. However, as you will have just awakened from anesthesia, you won’t be allowed to drink water freely at first—some patience will be needed.
- In a routine recovery, you will be transferred to your room in the ward around the 24th hour after surgery (this may vary depending on your condition).
- Once you are transferred to your room, you will be able to take care of your personal hygiene and walk around. Bed rest is not necessary; on the contrary, you are encouraged to sit up and perform breathing exercises.
- On the 5th day, you will be allowed to take a full-body shower.
- During your 5-day hospital stay, your condition will be monitored through specific blood tests and radiological examinations.
- When it’s time for discharge, you will be given detailed instructions about your medications, including a schedule specifying the exact times each should be taken.
- Do not try to recreate a hospital-like environment at home. Wake up at your usual time in the morning and make sure to walk frequently around the house. You can receive visitors, but avoid contact with individuals who are sick or may carry infections.
- Begin with short and slow walks outdoors, and gradually increase both the distance and pace each day to improve your physical conditioning.
- You may resume sexual activity starting from the first week after surgery.
- You will have an outpatient clinic appointment one week after being discharged from the hospital. During this visit, your surgical site and medications will be reviewed. After one week of regular walking, you may return to work in the third week, depending on your recovery.